By using our site you are consenting to their use, view more in our Cookie Policy.
When To Prescribe A Custom Orthotic
We will be running a monthly blog covering all things orthotics and biomechanics. To kick things off we will start with when to prescribe an orthotic. Please do give us feedback and recommendations of topics you’d like covering along the way.
When to prescribe an orthotic
I hate to break it to you but unfortunately there is no golden rule regarding when you should prescribe an orthotic. Realistically there are many factors which contribute to this decision-making process and not all are down to your clinical judgement…there are also many socioeconomic factors at play.
Clinically, you must consider the question: WHY do we prescribe orthotics?
What is their intended function? How will an orthotic help this individual?
Well, here is a bit of physics for you. An orthotic is designed to:
- Alter the location, vector and timing of forces at the foot orthoses interface
How do they do this I hear you ask. Through:
- Surface geometry – contouring
- Load/deformation characteristics - density
- Functional characteristics
So, to simplify, orthoses can alter loads on the body – where the load goes, when the load is applied, how much load goes where.
Take a look at the diagram below:
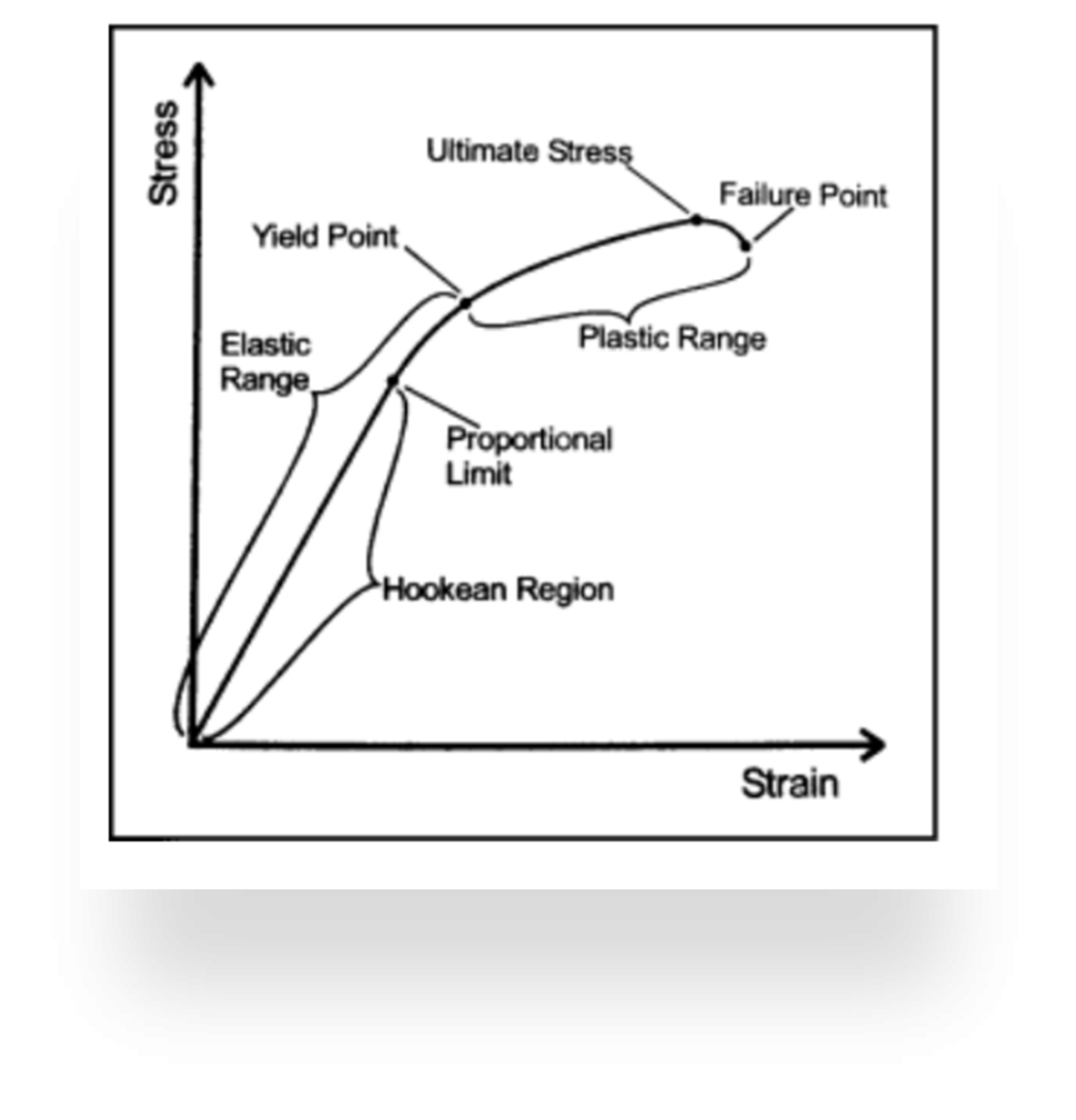
Mueller MJ, Maluf KS. Tissue adaptation to physical stress: a proposed “physical stress theory” to guide physical therapist practice, education, and research. Phys Ther. 2002;82:383– 403.
This is how the structures in our body respond to load.
- Stress = force/unit area due to an applied load
- Strain= physical deformation of a material in response to applied stress
Let’s apply this to the tibialis posterior tendon in PTTD.
In the elastic range, stress is applied to the tendon, the tendon elongates, but once the stress is removed the structure will return to normal.
Once the amount of stress to the tendon reaches beyond the yield point into the plastic range, the tendon will have experienced some sort of damage.
If even more stress is applied to reach the ultimate stress point, the tendon will fail, and we have our end stage of PTTD.
So, in this scenario we want to reduce the load going into the tibialis posterior tendon and we can do this with an orthotic!
YOUR JOB
Through patient history and biomechanical assessments, you need to:
- Identify the structure/s being excessively stressed
- Determine whether the aetiology of the patient's complaint is secondary to excessive mechanical loading (not neurological, vascular etc)
- Institute a management protocol which emphasizes: A) reducing tissue stress to a tolerable level; B) healing the involved tissues; and C) the restoration of flexibility and muscle strength to permit the resumption of daily activities
TISSUE STRESS THEORY McPoil and Hunt (1995)
Now think to yourself, what orthotic additions, modifications, materials, characteristics etc do I have available to me and will any of them help to reduce the stress on this structure…
If the answer is yes…then prescribe an orthotic!
But hold your horses, this is just from a clinical point of view. What about all those socioeconomic factors. From speaking to the patient, what are their expectations, are they sceptical, are they on board, would they wear them, will they fit in with their lifestyle and so on….
More on setting patient expectations in my next blog. Stay tuned!
